Abstract
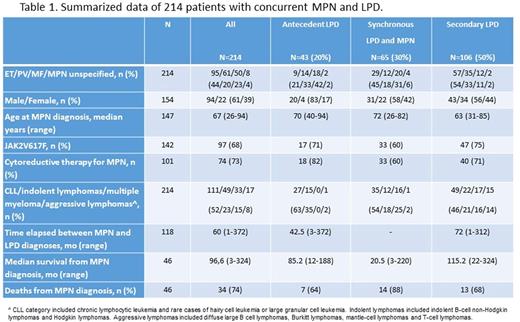
Patients with a Ph-negative myeloproliferative neoplasms (MPN) harbor or develop lymphoproliferative disorders (LPD) at a higher rate than general population and a common oncogenic pathway for MPN and LPD has been hypothesized, based on the presence of JAK2 V617F mutation in lymphocytes of patients with the concurrent diseases. Selected therapies for MPN might favor LPD, however, no large scale epidemiologic study ever specifically addressed this issue. We, therefore, conducted a scoping review of published literature in order to sum up the available evidence. We enquired EMBASE, PubMed and Cochrane Library and retrieved 2,064 English language full papers: 83 ones were selected and 62 full texts were definitely analyzed: 2 independent researchers extracted single-patient data for concurrent MPN and LPD cases and references were checked. Single-patient data were retrieved by 50 papers reporting 214 individuals with MPN and LPD: details are reported in Table 1. Half of the reported LPD cases occurred in the follow-up of diagnosed MPN (secondary LPD, sLPD) while 30% of the diagnoses were synchronous and 20% antecedent: indolent LPD occurred in 75% of the patients, while aggressive lymphomas in 8%. As compared with published MPN cohorts (Tefferi et al 2014 Blood), the patients showed a higher male-to-female ratio (1.56), an older age at MPN diagnosis, a lower portion of PV and a higher frequency of JAK2V617F mutation than expected, based on the frequency of PV cases. The patients also showed a high frequency of cytoreductive therapy and a shorter median survival (8 year) than expected. As compared with antecedent or synchronous LPDs, specific epidemiologic features were observed: sLPD cases more frequently occurred in the follow-up of patients with essential thrombocytemia (ET) than polycythemia vera (PV) or myelofibrosis (MF) (p<0.001), which is the probable reason for a lower median age at MPN diagnosis (63 versus 71 years, p<0.001) and a lower male-to-female ratio (1.27 vs 1.96, p=0.18). Nevertheless, V617F JAK2 mutation was harbored by the vast majority of sLPD cases, in particular, 83% of MF patients incurring sLPD carried the mutation (p=0.05). An even more impressive distinguishing feature of sLPD was the higher portion of aggressive lymphomas than reported for antecedent or synchronous LPD (14.1% versus 1.8%; p=0.004). Finally, due to the long time elapsed from MPN to LPD diagnoses, median survival of sLPD (9.6 years) was not significantly different from the overall cohort, but it was still shorter than the expected. A peculiar observation was also made relatively to patients with synchronous diagnosis of LPD and MPN: based on the survival data reported for 46 patients, they showed a sensibly dismal prognosis possibly due to lower intensity of therapeutic approaches, sustained by their old and the lack of therapies being effective both against MPN and LPD.
This thorough review of published evidence demonstrates that LPD are relevant clinical events in the history of MPN patients. LPD, including aggressive lymphomas, may occur in the follow-up of younger and/or ET patients, especially those harboring the V617FJAK2 mutation. Prospective interventional studies might not capture the risk of LPD due to the limited size of the studies and the short follow-up. Controlled studies are needed to better refine the target population at high risk of developing LPD in order to support surveillance programs and to avoid therapies (including JAK 2 inhibitors) possibly favoring LPD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal